Pain Modulation Currents
↵
Pain modulation
Pain
is unpleasant sensation of the body. The receptors of pain are called
nociceptors. Nociceptors are present all over the body especially skin
(subcutaneously). Any physical, thermal and mechanical pressure
stimulates the nociceptors.
The impulses are carried by two types of neuron; Primary or 1st order neuron and Secondary or 2nd order neuron.
1st order neuron:
2nd order neuron:
2nd order afferent fibers carry sensory impulses from the dorsal horn of the spinal cord to the brain.
- A α and A β are large diameter (myelinated) nerve fibers.
- A Δ and C fibers are the small diameter (unmyelinated) nerve fibers.
The
impulses from spinal cord to the brain are carried by Dorsal
spinothalamic tract, spinoreticular tract and spinocephalic tract.
Pain Gate Control Theory:
This theory was suggested by Pat wall and Melazak in 1965.
Afferent
input is mainly through posterior root of spinal cord and all afferent
information must pass through synapses in the Substantia Gelatinosa and
Nucleus Propius of the posterior horn.
Mechanism:
It
was suggested that pain to pass through this gate, there must be
unopposed passage for nociceptive information arriving at the synapse.
However if the gate is concurrently receiving the impulses produce by
the stimulation of large diameter fiber (thermoceptors, mechanoceptors).
Then this traffic predominates with the resultant presynaptic
inhibition of the small diameter nociceptive information. Many
physiotherapeutic agents causing stimulation of the endings connected to
the large diameter nerve fibers. The use of Manipulation, TENS,
Interferential therapy, Heat, Massage, Ice, Vibration and Movements can
produce reduction of pain by closing the pain gate.
1-Transcutaneous Electrical Nerve Stimulation (TENS)
It
is the application of low frequency pulsed rectangular current through
skin to reduce pain. A small battery machine is used to generate a
current having specific stimulatory effect.
Parameters of TENS:
Pulse shape: Rectangular
Pulsed width: Measured in microseconds and often 100 μs or 200 μs
Pulse frequency: As low as 2 Hz and as high as 600 Hz but usually fixed i.e. 150 Hz.
- High TENS: High frequency and low intensity
Frequency 100 – 500 Hz
Pulse width 100 – 500 μs
Intensity 5 – 30 mA
- Low TENS: Low frequency and high intensity
Frequency 1 -5 Hz
Pulse width 100 – 250 μs
Intensity more than 30 mA
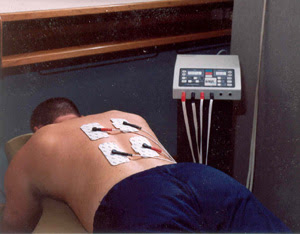
Electrode placement:
- Area of greater intensity of pain/near
- Trigger or motor point
Advantages of TENS:
- It is non – invasive, portable and non addictive.
- It is cheaper than regular analgesics.
- It has few contraindications and precautions
- It has changeable battery and electrodes.
Disadvantages of TENS:
- Number of patients fails to tolerate the electrical stimulation.
- Skin irritation may occur due to allergic reaction.
- Chemical burn is also a disadvantage of TENS.
Indications of TENS:
- Chronic pain syndrome
- Phantom limb pain
- Reflex sympathetic dystrophy
- Post operative conditions
- Obstetric pain
Contra indications:
- Continuous TENS may result some electrolytic reaction below the skin
- Pacemakers
- First three month of pregnancy
- Hemorrhagic conditions
- Open wounds
- Carotid sinus
- Over mouth
- Near eyes
Treatment method:
A patient may have a single daily treatment of 40 min duration. Portal TENS can be used continuously for 24 hrs.
Modes of TENS:
a. Conventional TENS:
It is the most commonly used mode of TENS. It can be used for both Acute and Chronic pain.
Mechanism of Action:
Stimulation of large diameter through pain gate control theory
- Frequency 100 – 150 Hz
- Intensity 12 – 30 mA
- Pulse width 50 – 80 µs
b. Acupuncture like mode:
Mechanism of Action:
The stimulation of small diameter nerve fibers to release endogenous opiods
Parameters:
- Frequency 1 -5 Hz
- Intensity above 30 mA
- Pulse duration 150 – 300 µs
c. Burst mode:
This mode has characteristics of both high and low TENS. The pain control is through both routes.
Parameters:
- Frequency 50 – 100 Hz but the frequency is delivered in packets of 1 – 4 Hz
- Pulse duration of 50 – 100 µs
- Intensity below 30 mA
d. Brief intense TENS:
It has rapid onset but for short term. Clinician used it for wound debridment, joint mobilization and contracture.
- Frequency 80 – 150 Hz
- Pulse duration 50 – 250 µs
- Intensity according to tolerance of patient
2-Interferential Current
Interferential
therapy was developed by Dr. Hans Nemec in 1950. It was suggested that
the use of two medium frequencies has the advantage of reducing skin
resistance.
Z = 1/2πfC
Where Z = Impedance
f = frequency
C = capacitance
When
the frequency increases the skin resistance decreases. So the
interferential therapy is used to treat the deep pain, idiopathic pain,
relieve edema, control stress incontinence (inability to control urine)
by stimulating pelvic floor muscles.
The
current is produced by mixing two medium frequency currents delivered
to skin through two sets of electrodes through separate channels in the
same stimulator. One current is normally of fixed frequency i.e. 5000 Hz
while the other frequency is variable i.e. 5200 Hz. The two alternating
currents interact with each other. When they are in the same phase
higher amplitude is produced and lower amplitude is produced when the
currents are in opposite phase. The interaction of two medium frequency
currents produce envelops of pulses known as beat frequency. Beat
frequency will be the subtraction of the two medium frequencies.
Physiological effects:
I. Pain relief:
The
increase in the blood circulation which may be produced by either
pumping effect of the stimulated muscles or the effect on the autonomic
nerves of blood vessels and therefore remove the chemicals from the area
which stimulates nociceptors. Low frequency currents with short
duration (at frequency of 100 Hz (5200 – 5100)) stimulate large diameter
nerve fibers which will have and affect on the pain gate and inhibition
of transmission of small diameter nociceptive traffic.
In
order to selectively activate the descending pain suppression system
with a frequency of 15 Hz (5200 – 5185) which stimulate small diameter
fibers eventually will cause the release of endogenous opiods.
II. Motor stimulation:
Normal
innervated muscle will be made to contract if the interferential
therapy is 1 – 100 Hz is used. The type of contraction depends upon the
frequency stimulation. At 1 – 5 Hz tickling (minimal contraction)
sensation is produced. Muscle twitch is produced at 5 – 20 Hz. Partial
tetanic contraction is produced from 20 Hz up to 30 Hz. And from 30 –
100 Hz complete tetanic contraction is produced.
The complete range of all contraction will be produced when rhythmical frequency between 1 – 100 Hz is used.
III. Removal of exudates:
Exudates
is accelerated by a frequency of 1 – 10 Hz with rhythmical pumping
action is produced by muscle contraction and therefore is possibly an
effect on autonomic nervous nerves which can affect the diameter of
blood vessels and therefore increased blood circulation. Both factors
help in the removal of exudate.
Indications of Interferential therapy:
1. Pain:
It
is useful in wide variety of painful conditions (Acute, Chronic, Deep,
Idiopathic, Subacute pains etc) AMF (Amplitude Modulating Frequency) 70 –
150 Hz is used for Acute Pain. Frequency below 50 Hz is used for
chronic pain and subacute pain where muscle contraction is required.
2. Oedema:
Frequency of 1 – 10 Hz is used for to reduce oedema i.e. oedema of hand and feet.
3. Stress incontinence:
Quadripolar technique:
Two
electrodes are placed on lower abdomen while the other two are placed
on inner upper thigh. This technique is used in stress incontinence.
Contra – indications:
- Pace maker
- Pregnancy
- On chest wall in cardiac patients
- Hemorrhage
- Malignancy
- Skin infection
- Deep vein thrombosis













Comments
Post a Comment